Introducing Stedi’s Payers API
Sep 24, 2024
Products
Every clearinghouse maintains a list of supported payers, supported transaction types, and other key integration details. The problem? This vital information is typically provided in a CSV file over email and updated monthly at best. Worse, updated payer lists often contain breaking changes, duplicate payer names, and typos that cause failed transactions and endless code rewrites.
Instead of a static payer list, we built the world’s most developer-friendly payer database: the Stedi Payer Network, which is uniquely designed to help you build more efficient and reliable integrations with thousands of medical and dental payers. It’s just one of the ways Stedi's clearinghouse gives modern healthcare companies the developer experience, security, and reliability they need to build world-class products for providers and patients.
Stable, unified payer records
Every EHR system and clearinghouse uses payer IDs to route transactions to payers. It can be hard to know which ID to use for requests because payer IDs vary between clearinghouses, and some clearinghouses assign separate IDs to different transactions with the same payer. Once you determine the right ID, frequent payer list updates require tedious remapping in your codebase.
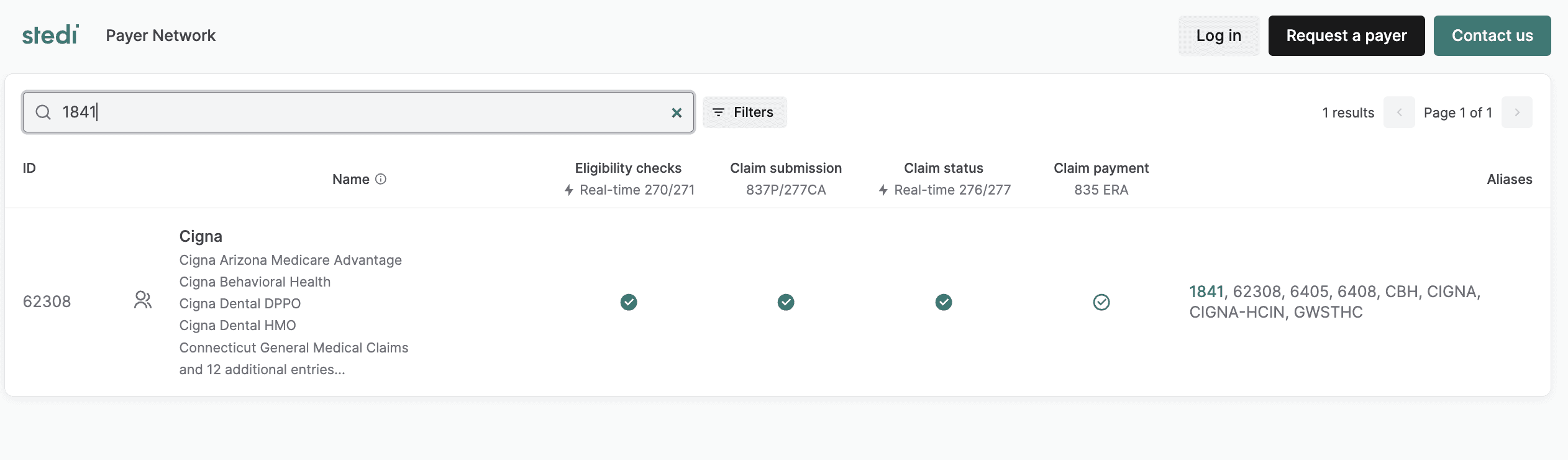
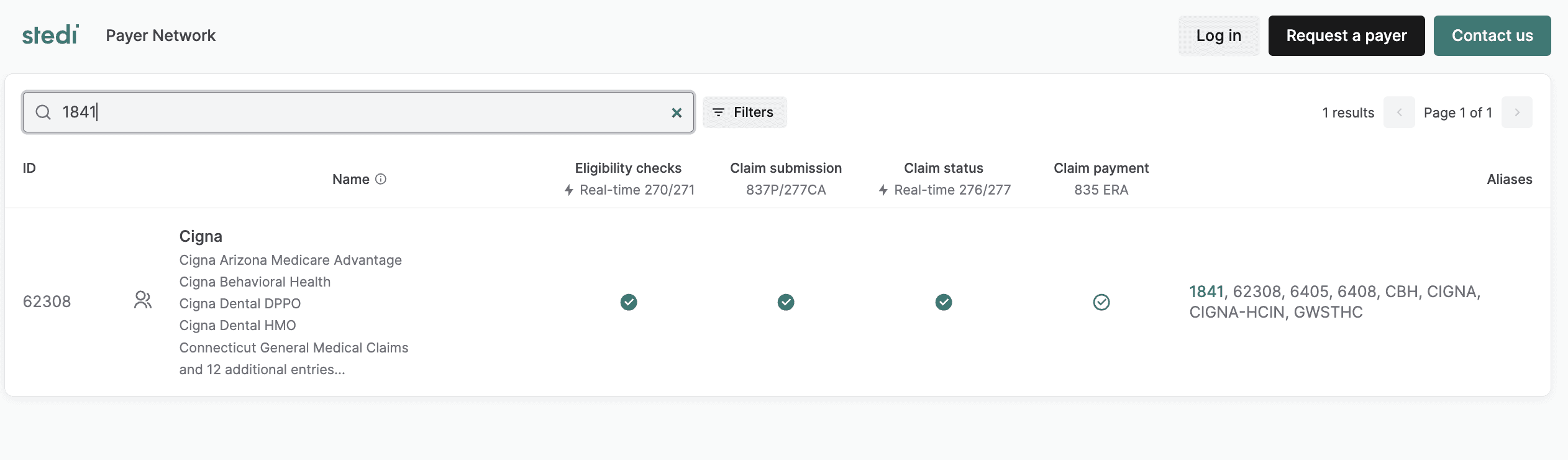
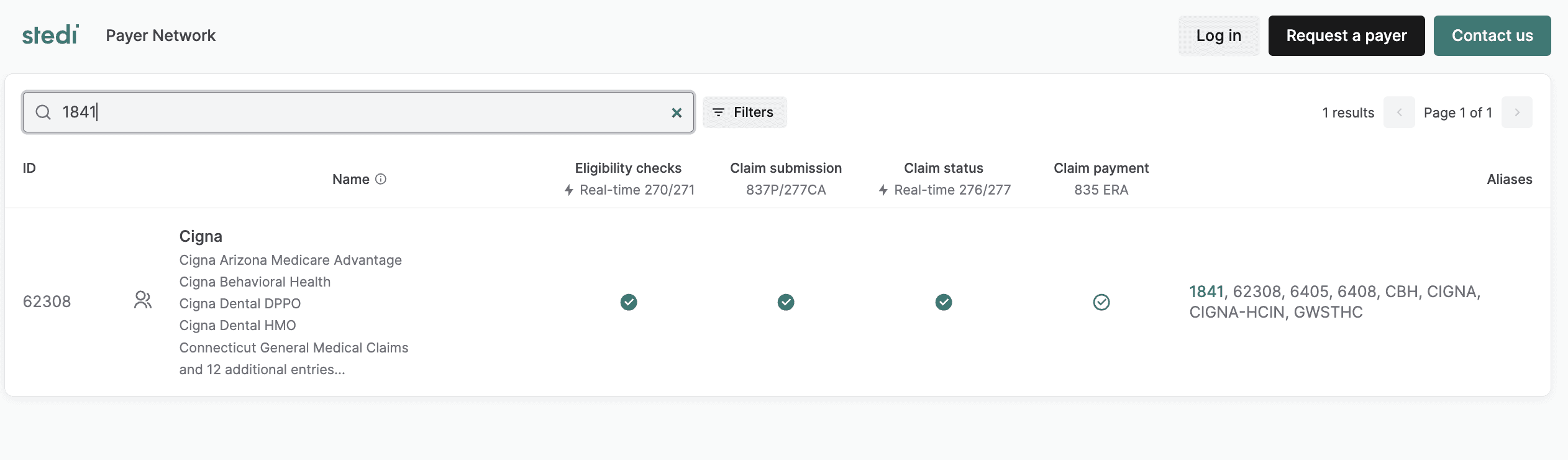
The Stedi Payer Network eliminates this problem by mapping all of a payer’s commonly used names and IDs (aliases) to a single payer record, and Stedi automatically uses the required ID for the payer on the backend. For example, searching our interactive network page by any of Cigna’s aliases, such as 1841, CIGNA, and GWSTHC returns the same result, even though the most common Payer ID for Cigna is 62308.
This approach means Stedi likely already supports all of the common payer IDs you use today, making it easy to migrate to Stedi from other clearinghouses. And if you need a new alias for any existing payer, just let us know and we’ll add it to the network the same day.
Programmatic access to real-time updates
With the List Payers API, developers can retrieve Stedi’s complete, production payer list in seconds for use in any system or application. For example, you can:
Embed Stedi’s payer list within a patient intake form, allowing patients to choose from a list of supported payers.
Build simpler EHR integrations using the payer IDs in the provider’s EHR.
Create nightly or real-time syncs between your internal payer list and Stedi’s payer list.
Migrate or reroute transactions to Stedi’s clearinghouse without dynamically changing payer IDs.
The following Blue Cross Blue Shield of North Carolina response example shows that real-time eligibility checks, real-time claim status requests, and professional claims are supported for this payer. The response also indicates that payer enrollment is required for 835 ERAs (claim remittances).
{ "stediId": "UPICO", "displayName": "Blue Cross Blue Shield of North Carolina", "primaryPayerId": "BCSNC", "aliases": [ "1411", "560894904", "61473", "7472", "7814", "BCBS-NC", "BCSNC", "NCBCBS", "NCPNHP" ], "names": [ "Blue Cross Blue Shield North Carolina" ], "transactionSupport": { "eligibilityCheck": "SUPPORTED", "claimStatus": "SUPPORTED", "claimSubmission": "SUPPORTED", "claimPayment": "ENROLLMENT_REQUIRED" } }
Broad, reliable connectivity
Stedi already supports thousands of medical and dental payers, and we add more every week. Here are the number of unique payers supported for specific transaction sets:
Real-time eligibility checks - 1,100+ unique payers
Claim submissions - 2,700+ unique payers
Real-time claim status requests - 300+ unique payers
835 ERAs (claim remittances) - 1,800+ unique payers
On the backend, Stedi has multiple, redundant routes to payers through a combination of direct payer integrations and connectivity through intermediary clearinghouses. Whenever possible, Stedi automatically routes requests and responses to the most reliable connection, increasing uptime and reliability across the network.
You get redundancy and reliability with no additional effort or cost when you integrate with Stedi – we manage all of the payer routing logic seamlessly behind the scenes. We add new payers daily, so feel free to request new payers or new transaction types for an existing payer.
Get started with Stedi
Stedi’s programmatically accessible payer network is one of the many ways our clearinghouse accelerates payer integration.
"The speed at which we got up and running in production with Stedi was remarkable. From the moment we began integration, it was clear that Stedi was designed with user ease and efficiency in mind.”
- Chris Parker, Chief Technology Officer PQT Health
Contact us to speak to the team and learn how Stedi can help you automate and simplify your eligibility and claims workflows. And if you want to see what percentage of your payer list we support, we’d be happy to do the comparison for you.
Every clearinghouse maintains a list of supported payers, supported transaction types, and other key integration details. The problem? This vital information is typically provided in a CSV file over email and updated monthly at best. Worse, updated payer lists often contain breaking changes, duplicate payer names, and typos that cause failed transactions and endless code rewrites.
Instead of a static payer list, we built the world’s most developer-friendly payer database: the Stedi Payer Network, which is uniquely designed to help you build more efficient and reliable integrations with thousands of medical and dental payers. It’s just one of the ways Stedi's clearinghouse gives modern healthcare companies the developer experience, security, and reliability they need to build world-class products for providers and patients.
Stable, unified payer records
Every EHR system and clearinghouse uses payer IDs to route transactions to payers. It can be hard to know which ID to use for requests because payer IDs vary between clearinghouses, and some clearinghouses assign separate IDs to different transactions with the same payer. Once you determine the right ID, frequent payer list updates require tedious remapping in your codebase.
The Stedi Payer Network eliminates this problem by mapping all of a payer’s commonly used names and IDs (aliases) to a single payer record, and Stedi automatically uses the required ID for the payer on the backend. For example, searching our interactive network page by any of Cigna’s aliases, such as 1841, CIGNA, and GWSTHC returns the same result, even though the most common Payer ID for Cigna is 62308.
This approach means Stedi likely already supports all of the common payer IDs you use today, making it easy to migrate to Stedi from other clearinghouses. And if you need a new alias for any existing payer, just let us know and we’ll add it to the network the same day.
Programmatic access to real-time updates
With the List Payers API, developers can retrieve Stedi’s complete, production payer list in seconds for use in any system or application. For example, you can:
Embed Stedi’s payer list within a patient intake form, allowing patients to choose from a list of supported payers.
Build simpler EHR integrations using the payer IDs in the provider’s EHR.
Create nightly or real-time syncs between your internal payer list and Stedi’s payer list.
Migrate or reroute transactions to Stedi’s clearinghouse without dynamically changing payer IDs.
The following Blue Cross Blue Shield of North Carolina response example shows that real-time eligibility checks, real-time claim status requests, and professional claims are supported for this payer. The response also indicates that payer enrollment is required for 835 ERAs (claim remittances).
{ "stediId": "UPICO", "displayName": "Blue Cross Blue Shield of North Carolina", "primaryPayerId": "BCSNC", "aliases": [ "1411", "560894904", "61473", "7472", "7814", "BCBS-NC", "BCSNC", "NCBCBS", "NCPNHP" ], "names": [ "Blue Cross Blue Shield North Carolina" ], "transactionSupport": { "eligibilityCheck": "SUPPORTED", "claimStatus": "SUPPORTED", "claimSubmission": "SUPPORTED", "claimPayment": "ENROLLMENT_REQUIRED" } }
Broad, reliable connectivity
Stedi already supports thousands of medical and dental payers, and we add more every week. Here are the number of unique payers supported for specific transaction sets:
Real-time eligibility checks - 1,100+ unique payers
Claim submissions - 2,700+ unique payers
Real-time claim status requests - 300+ unique payers
835 ERAs (claim remittances) - 1,800+ unique payers
On the backend, Stedi has multiple, redundant routes to payers through a combination of direct payer integrations and connectivity through intermediary clearinghouses. Whenever possible, Stedi automatically routes requests and responses to the most reliable connection, increasing uptime and reliability across the network.
You get redundancy and reliability with no additional effort or cost when you integrate with Stedi – we manage all of the payer routing logic seamlessly behind the scenes. We add new payers daily, so feel free to request new payers or new transaction types for an existing payer.
Get started with Stedi
Stedi’s programmatically accessible payer network is one of the many ways our clearinghouse accelerates payer integration.
"The speed at which we got up and running in production with Stedi was remarkable. From the moment we began integration, it was clear that Stedi was designed with user ease and efficiency in mind.”
- Chris Parker, Chief Technology Officer PQT Health
Contact us to speak to the team and learn how Stedi can help you automate and simplify your eligibility and claims workflows. And if you want to see what percentage of your payer list we support, we’d be happy to do the comparison for you.
Every clearinghouse maintains a list of supported payers, supported transaction types, and other key integration details. The problem? This vital information is typically provided in a CSV file over email and updated monthly at best. Worse, updated payer lists often contain breaking changes, duplicate payer names, and typos that cause failed transactions and endless code rewrites.
Instead of a static payer list, we built the world’s most developer-friendly payer database: the Stedi Payer Network, which is uniquely designed to help you build more efficient and reliable integrations with thousands of medical and dental payers. It’s just one of the ways Stedi's clearinghouse gives modern healthcare companies the developer experience, security, and reliability they need to build world-class products for providers and patients.
Stable, unified payer records
Every EHR system and clearinghouse uses payer IDs to route transactions to payers. It can be hard to know which ID to use for requests because payer IDs vary between clearinghouses, and some clearinghouses assign separate IDs to different transactions with the same payer. Once you determine the right ID, frequent payer list updates require tedious remapping in your codebase.
The Stedi Payer Network eliminates this problem by mapping all of a payer’s commonly used names and IDs (aliases) to a single payer record, and Stedi automatically uses the required ID for the payer on the backend. For example, searching our interactive network page by any of Cigna’s aliases, such as 1841, CIGNA, and GWSTHC returns the same result, even though the most common Payer ID for Cigna is 62308.
This approach means Stedi likely already supports all of the common payer IDs you use today, making it easy to migrate to Stedi from other clearinghouses. And if you need a new alias for any existing payer, just let us know and we’ll add it to the network the same day.
Programmatic access to real-time updates
With the List Payers API, developers can retrieve Stedi’s complete, production payer list in seconds for use in any system or application. For example, you can:
Embed Stedi’s payer list within a patient intake form, allowing patients to choose from a list of supported payers.
Build simpler EHR integrations using the payer IDs in the provider’s EHR.
Create nightly or real-time syncs between your internal payer list and Stedi’s payer list.
Migrate or reroute transactions to Stedi’s clearinghouse without dynamically changing payer IDs.
The following Blue Cross Blue Shield of North Carolina response example shows that real-time eligibility checks, real-time claim status requests, and professional claims are supported for this payer. The response also indicates that payer enrollment is required for 835 ERAs (claim remittances).
{ "stediId": "UPICO", "displayName": "Blue Cross Blue Shield of North Carolina", "primaryPayerId": "BCSNC", "aliases": [ "1411", "560894904", "61473", "7472", "7814", "BCBS-NC", "BCSNC", "NCBCBS", "NCPNHP" ], "names": [ "Blue Cross Blue Shield North Carolina" ], "transactionSupport": { "eligibilityCheck": "SUPPORTED", "claimStatus": "SUPPORTED", "claimSubmission": "SUPPORTED", "claimPayment": "ENROLLMENT_REQUIRED" } }
Broad, reliable connectivity
Stedi already supports thousands of medical and dental payers, and we add more every week. Here are the number of unique payers supported for specific transaction sets:
Real-time eligibility checks - 1,100+ unique payers
Claim submissions - 2,700+ unique payers
Real-time claim status requests - 300+ unique payers
835 ERAs (claim remittances) - 1,800+ unique payers
On the backend, Stedi has multiple, redundant routes to payers through a combination of direct payer integrations and connectivity through intermediary clearinghouses. Whenever possible, Stedi automatically routes requests and responses to the most reliable connection, increasing uptime and reliability across the network.
You get redundancy and reliability with no additional effort or cost when you integrate with Stedi – we manage all of the payer routing logic seamlessly behind the scenes. We add new payers daily, so feel free to request new payers or new transaction types for an existing payer.
Get started with Stedi
Stedi’s programmatically accessible payer network is one of the many ways our clearinghouse accelerates payer integration.
"The speed at which we got up and running in production with Stedi was remarkable. From the moment we began integration, it was clear that Stedi was designed with user ease and efficiency in mind.”
- Chris Parker, Chief Technology Officer PQT Health
Contact us to speak to the team and learn how Stedi can help you automate and simplify your eligibility and claims workflows. And if you want to see what percentage of your payer list we support, we’d be happy to do the comparison for you.
Share
Get started with Stedi
Get started with Stedi
Automate healthcare transactions with developer-friendly APIs that support thousands of payers. Contact us to learn more and speak to the team.
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Developers
Resources
Backed by
Stedi and the S design mark are registered trademarks of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Developers
Resources
Backed by
Stedi and the S design mark are registered trademarks of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Developers
Resources
Get updates on what’s new at Stedi
Backed by
Stedi and the S design mark are registered trademarks of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
