Claim validation
Stedi's database of edits and repairs mean fewer payer rejections and faster payments.
New claim edits weekly
Our edits cover all SNIP Types. Check our changelog for the latest. Request a new edit.
Track outstanding claims
Keep providers informed with claim acknowledgments and real-time claim status updates.
Ingest ERAs
Automatically ingest electronic remittances (ERAs) to reconcile payments faster.
How it works
Integrate with a modern, developer-friendly API
Claim submission
Submit Professional (837P), Dental (837D), and Institutional (837I) claims to thousands of payers. Stedi creates a HIPAA-compliant transaction, applies enhanced edits, and sends it to the right payer.
submitClaim.js
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
getClaimStatus.js
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
Real-time claim status
Check any claim’s status in seconds with our JSON-based Claim Status API or the Stedi portal.
Electronic remittance advice (ERAs)
Receive ERAs automatically through Stedi webhooks or periodically poll for new transactions.
Use the Stedi portal or our API to get your ERAs as PDFs. Use the PDFs to post remittances by hand or keep a physical copy of your ERAs.
electronicRemittanceAdvice.json
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
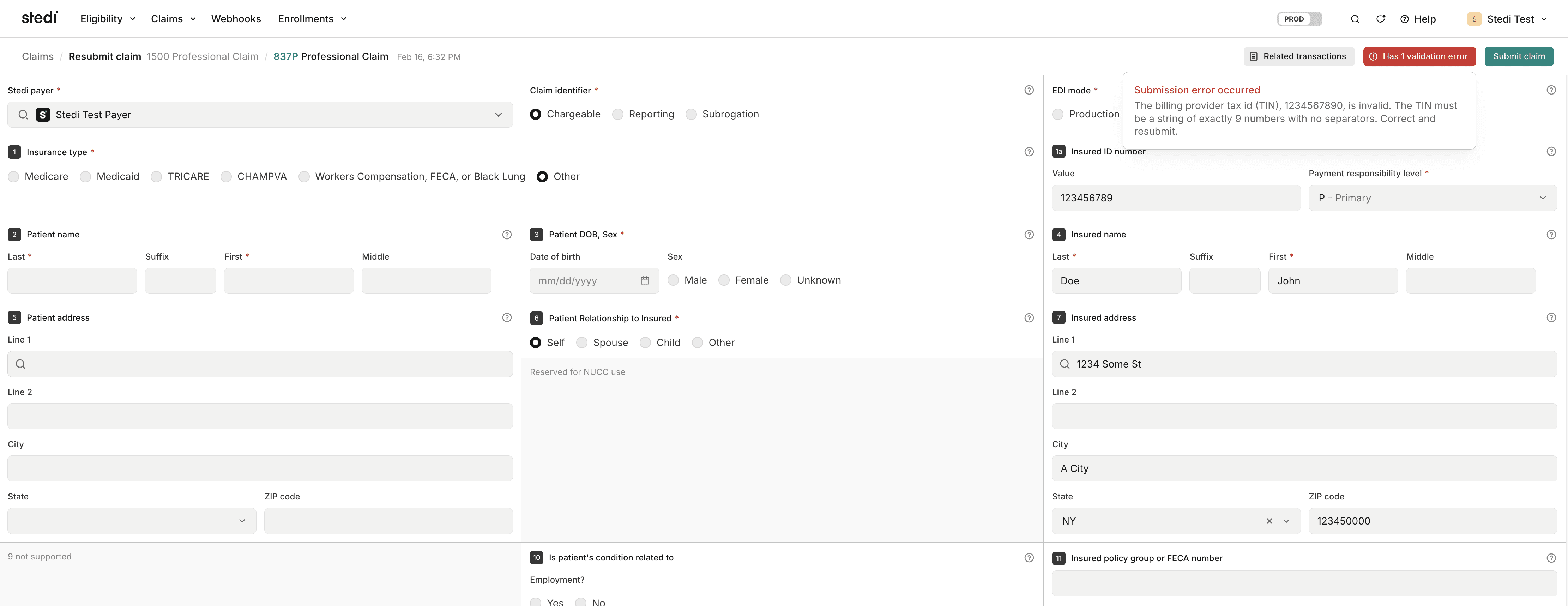
Built-in claim validation
Stedi validates every claim you submit against an extensive database of edits and repairs. These validation rules catch – and, where possible, fix – errors before they reach the payer. That means fewer payer rejections, which means faster payment.
Our edits cover all SNIP Types, including payer-specific SNIP Type 7 edits. We ship new edits weekly. See our changelog for the latest.
claimEditError.json
1
2
3
4
5
6
7
8
9
Manual claim submission
Test integrations and review claims in a familiar format
Submit professional claims through a digital version of the CMS-1500 claim form. Download auto-generated CMS-1500 PDFs through
the Stedi portal or API.
Connect to thousands of payers
Our growing set of payers provide broad, reliable connectivity.
Automatic failover
Stedi dynamically routes traffic to the most reliable connection, eliminating single points of failure, providing redundant connections.